The haze hung heavy over the Queen City as smoke from the Canadian wildfires crept into the Tristate. Fine particulates from the smoke, combined with summertime increases in ozone, created unhealthy conditions for people with heart and lung disease, children and older adults in late June 2023.
It was an eerie spectacle repeated in cities across the Midwest and Northeastern United States. Some skylines, like in New York City,
turned an almost apocalyptic shade of burnt orange as wildfire smoke made its way across the continent.
The smoke got a lot of people thinking about the air we breathe, and the impact air pollution, pollens and other allergens can have on our overall lung health. It's a conversation that's especially important for people managing asthma, COPD, and other chronic breathing and respiratory issues.
Overall air quality is improving in Greater Cincinnati
The
Southwest Ohio Air Quality Agency is tasked with monitoring our region's air quality for five major categories of pollutants: carbon monoxide, nitrogen dioxide, sulfur dioxide, ozone and particulate matter. Joy Landry, communications specialist for the agency, says the region's air has improved dramatically over the past 35 years.
“Two major improvements have helped: coal plants have mitigation processes to reduce sulfur dioxide and motor vehicles are required to meet U.S. EPA fuel efficiency standards," Landry explains. “Car manufacturers have used technology to improve engines and exhaust systems to burn fuel much cleaner."
Even with that progress, the Southwest Ohio Air Quality Agency keeps track of the air and issues alerts for anything that could impact health – like fine particulate matter from disasters such as wildfires to smog formed on hot summer days when pollutants react with sunlight to create ground-level ozone.
Air Quality Index and its Impact on Health
Results of how clean or dirty the air is get assigned a number from zero to 500 and reported as the Air Quality Index (AQI). Numbers from 50 and lower are Good. We enter the unhealthy territory once the AQI reaches 101 and higher.
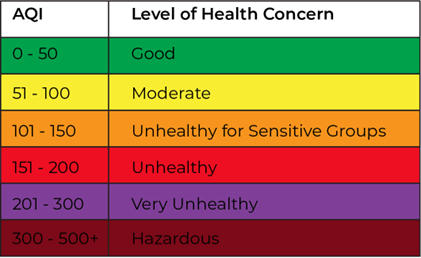
Image Source: Southwest Ohio Air Quality Agency
“Hot summer days with abundant sunshine, low winds, and little humidity or precipitation are ideal conditions for ozone formation," Landry says. “If elevated ozone concentrations are expected to reach an Air Quality Index over 101, we issue an Air Quality Alert to raise public awareness of poor air quality."
In the 101 – 150 range, the air is unhealthy for sensitive groups, which Landry says includes people with respiratory illnesses like asthma, young children, and senior citizens who may need to limit outdoor activities. At 151 and up, the general public may start experiencing effects of poor air quality.
Krishna Gannamraj, DO, a pulmonologist with The Christ Hospital Physicians, says people with jobs that carry occupational exposures to air pollutants need to be especially watchful when the AQI reaches unhealthy levels.
“People who are in welding, industrial chemicals, or anything like that, whenever they have worsened exposures, they do end up having exacerbations," Dr. Gannamraj says. “It can cause them to have increased shortness of breath, cough, and sputum production."
With wildfires in particular, the Centers for Disease Control says prolonged exposure can irritate the eyes, nose, throat, and lungs. Some particulate matter in wildfire smoke is microscopic – a fraction of the thickness of human hair and even smaller than common dust and pollen particles.
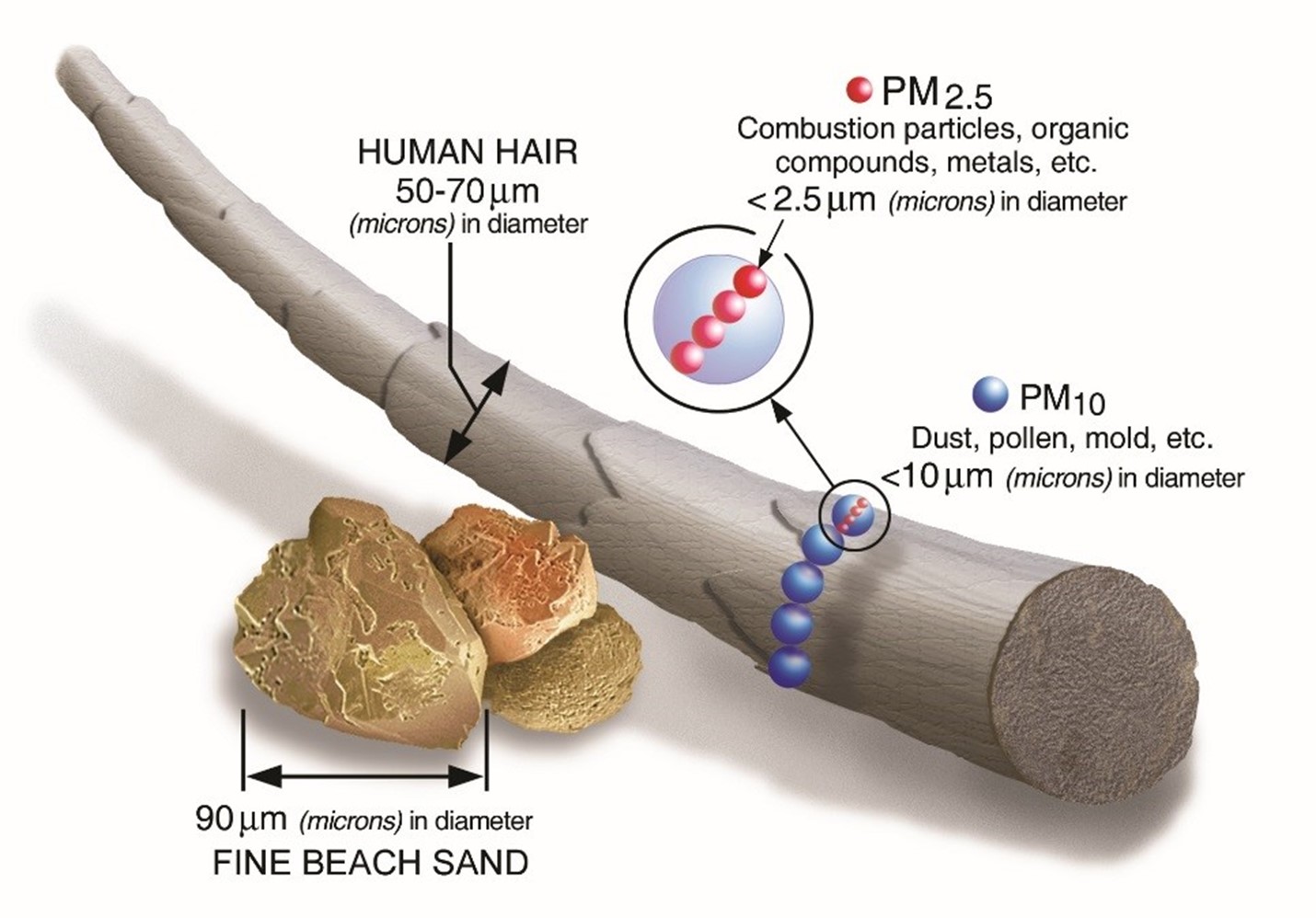
Source: U.S. EPA
Those particles are especially bad for your health because they can get deep into the lungs and possibly even into the bloodstream according to the U.S. EPA.
When wildfire smoke raises the local AQI, health experts recommend you limit outdoor activity and stay indoors. Keep your pets inside, too, because they can also be affected by wildfire smoke!
If you do need to be outside for an extended time when wildfire smoke is present, the CDC recommends wearing a tight-fitting NIOSH-approved N95 or P100 respirator. While cloth masks are good for limiting the spread of respiratory droplets that carry illnesses like the flu and COVID-19, the EPA says NIOSH-approved masks are better at reducing exposure to wildfire smoke.
Spring and fall bring more familiar air quality concerns
Pollutants aren't the only thing floating in the air that can make breathing miserable. Anyone with seasonal allergies knows that the influx of certain pollens, especially in spring and autumn, can trigger reactions. Respiratory viruses can add to the misery, especially for anyone with chronic lung conditions.
The Asthma and Allergy Foundation of America has gone as far as identifying the third week of September as one of the worst times of year for asthma attacks as several risk factors collide.
“This is typically the time of year when ragweed becomes prevalent," Landry says. Mold from falling leaves is also on the rise. Then you have more people spending more time indoors as summer activities draw to a close and children return to school.
“There are fewer respiratory viral infections in the summer compared to early fall, and those infections are honestly the most common cause of exacerbations," Dr. Gannamraj says. “When you're in a closed environment [like a classroom] and around other people, kids can bring respiratory tract infections home with them, then that is passed on to family members."
Staying on top of breathing issues year-round
Most healthy individuals will recover from allergies and respiratory illnesses with over-the-counter medicines and a little extra rest. Dr. Gannamraj says when certain symptoms linger, it's probably time to reach out to your primary care provider or consider virtual care options like a 24/7 Video Visit.
“Unremitting cough, fevers that are not going away, or sputum production that is a different color are signs that we need to keep an eye out for a respiratory tract infection," Dr. Gannamraj says.
For those with additional concerns about lung health, like asthma, COPD, or long COVID, there are steps you can take to protect your breathing no matter the time of year.
Keep up with the Air Quality Index
You can check the AQI online at AirNow.gov. The site provides reporting by Zip code and lets you know what pollutants are impacting air quality.
If you're primarily interested in pollen and mold, the Southwest Ohio Air Quality Agency posts daily counts on its website. It also offers the PollenWise app that you can download to your cell phone.
Wear a mask or face covering
Respiratory infections are one of the most common causes of asthma attacks and breathing issues, so one of the best things you can do is avoid getting sick in the first place.
Dr. Gannamraj recommends at-risk patients wearing a cloth or surgical mask around large groups of people.
“We found out during COVID that when people wore masks, we saw fewer cases of flu because people were more vigilant about wearing masks," Dr. Gannamraj says.
Quit smoking and vaping
Quitting smoking is great health advice for anyone, but especially for better lung health. Smoking and vaping are connected to developing lung diseases in the future.
“The thing I tell my COPD patients is the best way to help yourself is stopping smoking, because that's the number one way to make sure your lung function doesn't worsen," Dr. Gannamraj says.
If you are a tobacco user who is ready to quit, The Christ Hospital offers free smoking cessation resources.
Stay up to date on vaccines
Keeping up with vaccinations is another good measure for preventing respiratory infections, especially for those with lung diseases. Those include annual flu shots, COVID-19 vaccines and boosters, and pneumococcal vaccines for those who are eligible.
In addition to protecting yourself, Dr. Gannamraj says you're also protecting those around you. “Your family and friends who may not be as healthy as you may be more prone to developing severe infections," he says. “That's why it's very important for all of us to be very up to date on our vaccines."
Stay current with your maintenance medications
Maintenance medications are very beneficial to better breathing when taken as prescribed, but it's important to watch for changes like increased use of rescue inhalers.
“If you're starting to notice that you're having to wake up at night to use a rescue inhaler, or your more short of breath and using your rescue inhaler throughout the day, go ahead and message your doctor to see what's going on," Dr. Gannamraj says.
Patients may also want to talk to their primary care provider about being referred to a pulmonologist for specialized care if they are having exacerbations that are no longer being controlled.
“Not only can we titrate your inhaler therapy, we can also check your labs and see if there are other medications you may be qualified for," Dr. Gannamraj says. “There are a lot of new biologic medications that have been really beneficial and help patients avoid the use of oral steroids."