Getting enough sleep is an essential part of staying healthy. It's so important that we spend about a
third of our lives sleeping. Sleep apnea, however, causes an estimated 22 million people to wake up frequently at night, preventing them from getting the sleep they need.
If left untreated, sleep apnea can lead to several health complications that worsen over time. So it's important to detect and treat sleep apnea early. Joseph Hellmann, MD, an ear, nose and throat (ENT) specialist with The Christ Hospital Physicians, explains the signs and symptoms of sleep apnea and innovative treatment options to help you get restful sleep.
Sleep apnea cuts off airflow while you sleep
Sleep apnea refers to limited airflow due to a partial or complete blockage of the upper airway. It is often caused by muscles in the throat relaxing and limiting the airflow.
"That's why some people say they only snore after a few alcoholic beverages, for example. Alcohol relaxes the muscles," says Dr. Hellmann. "While muscles relax normally when we sleep, it can restrict airflow in certain cases."
Sleep apnea ranges from mild to severe, depending on how many times per hour your airflow is partially or completely blocked while sleeping.
- Normal: fewer than five events per hour
- Mild: five to 15 events per hour
- Moderate: 15 to 30 events per hour
- Severe: more than 30 events
Generally, doctors use a
sleep study to measure the number of blocked airflow events you have while sleeping and diagnose the severity of your sleep apnea.
People with sleep apnea usually have multiple causes
Sleep apnea is more common in people who are older and overweight. However, many things can obstruct airflow when you sleep.
Muscle function, tonsils, allergies, severe congestion or a more serious medical condition can all contribute. The physical structure of the roof of your mouth and jaw position can also contribute to blocking the upper airway. Sometimes, your sleep position can block airflow.
The standard of care for sleep apnea
Generally, doctors use three approaches to treat sleep apnea, ranging from least to most invasive:
- Treat reversible conditions, such as allergies, severe congestion or excess weight. Your doctor may also recommend changing your sleeping position or avoiding alcohol before bed.
- Introduce devices designed to keep the upper airway open while you sleep, such as a continuous positive airway pressure (CPAP) machine or oral appliance
- Use surgery if devices fail, such as surgery to remove tonsils or uvula.
New devices revolutionize sleep apnea care
Standard treatment options still have limitations. Surgery, for example, doesn't change anything about how your airway functions.
"The upper airway isn't a fixed pipe that stays open with surgical removal of tissues. While surgery to removing tonsils, for example, does create space, we're not changing anything about the upper airway itself. There's a lot of dynamic muscle activity that affects how the upper airway opens and closes. We can't change that with surgery." says Dr. Hellmann.
And while most people qualify for devices like CPAP, they may have a hard time wearing a mask at night. It's also hard to keep clean.
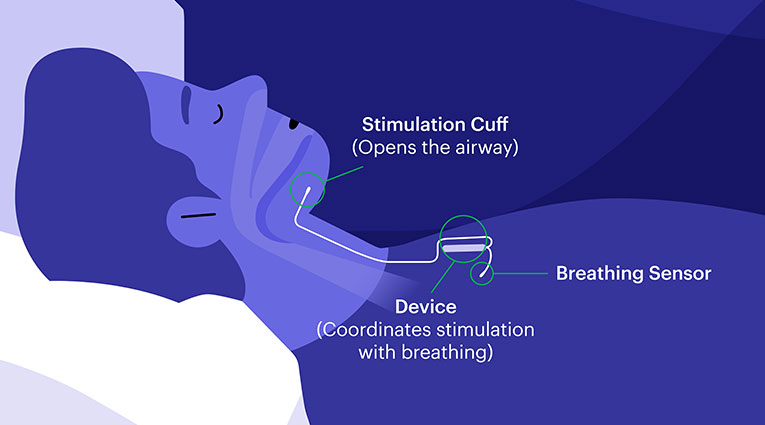
Dr. Hellmann has been one of the leading providers in the Greater Cincinnati area offering an innovative treatment called Inspire. This implantable device activates nerves that push the tongue and palate of your mouth forward each time you breathe. That movement keeps your airway open. As a result, it addresses the actual function of the airway, which surgical resection of tissues cannot address. And a bonus: you don't have to wear a mask while you sleep.
"Overall, Inspire is life changing. Though nothing is 100%, the success rate of this device is better than any treatment we've used in the past," says Dr. Hellmann.
Dr. Hellmann notes that you must meet the following criteria to qualify for Inspire:
- You must have tried other treatments, including a trial of CPAP
- You have a body mass index (BMI) less than 32 (people on Medicare must have a BMI under 34)
- You've had a sleep study done in the past two years showing you have between 15 and 65 partial or complete obstruction events each night while sleeping
- Be willing to complete a drug-induced sleep evaluation. First, a specialist will give you anesthesia to put you into a sleep state. Then, a doctor can examine your upper airway to make sure Inspire will help you.
The importance of treating sleep apnea early
"Sleep apnea is slow and insidious," says Dr. Hellmann. "At first, you may just notice that you're not sleeping well, so you feel more tired. But not getting enough sleep can also cause your cognitive functions to decline if you're constantly being partially awakened several times at night."
Untreated sleep apnea can also increase your risk of cardiovascular complications. Poor sleep quality can lead to high blood pressure, arrhythmias (abnormal heart rhythms), heart attacks, strokes and heart failure.
"Patients and providers are becoming more aware that sleep apnea can have significant repercussions on their cardiovascular health," says Dr. Hellmann. "It's important to keep raising this awareness."
When to see a doctor about sleep apnea
The most obvious signs of sleep apnea include loud snoring, often caused by a partial airway block. You may also wake up gasping for air if you experience a complete block. Over time, you may feel sluggish and tired when you wake up.
If you're concerned about sleep apnea, act now. Schedule an appointment with your primary care provider or consult with the
ENT specialists at The Christ Hospital Health Network. They work closely with sleep specialists to understand the root cause of your sleep apnea and use the latest technologies to help get you the sleep you need.